EnlargedProstate.jpg
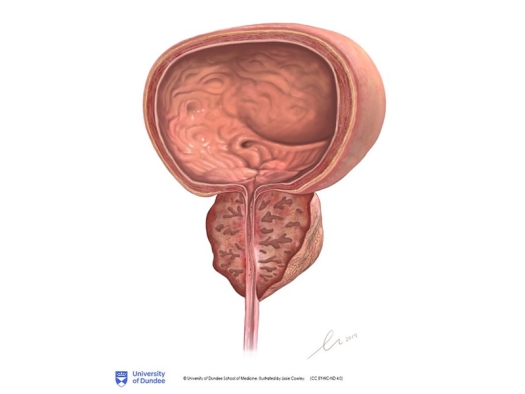
Illustration by Lissie Cowley, University of Dundee School of Medicine / CC BY-NC-ND 2.0
When treating a disease or a syndrome, it’s always important to treat the cause. The problem is that sometimes it’s difficult to find the cause. And then there are cases where there are multiple causes, all of which need to be accounted for. This is certainly true for cases of an enlarged prostate. There can be several factors at work in this condition. And one of the most common factors that can go ignored is metabolic syndrome. If this factor is overlooked, it may be impossible to have a successful outcome.
You probably already know that metabolic syndrome is incredibly common and is responsible in large part for cardiovascular disease, high blood pressure, cancer, and diabetes. But what you might not realize is that metabolic syndrome is also a big cause of BPH (prostate enlargement) and bladder symptoms. And, since metabolic syndrome in men is almost always associated with low testosterone, besides correcting the causes of metabolic syndrome, guess what therapy will often turn BPH around. So, if you are concerned about BPH symptoms, read on.
The authors of a new study point out that BPH and bladder symptoms in men are especially frequent in men who also have metabolic syndrome.
Metabolic syndrome includes a number of different factors, but the major factor is insulin resistance. Insulin resistance means that the cells no longer respond to the hormone insulin. This causes the body to compensate by increasing the production of insulin often to very high levels. It is these high levels of insulin that cause the metabolic imbalances that ultimately result in most of the symptoms associated with metabolic syndrome.
A 2012 paper determined that close to an incredible 35% of Americans had metabolic syndrome. By now, 10 years later, I am sure that this number is much higher. So what do high insulin levels have to do with BPH?
The study I just mentioned found that fasting blood insulin levels were “an independent risk factor for increased prostate gland volume.” The patients who had fasting plasma insulin levels less than 7 mU/mL, had an annual prostate growth rate of 0.84 mL per year while those with fasting plasma insulin levels >13 mU/mL had an annual prostate growth rate of 1.49 mL per year – almost twice as much! Here’s why this is important. A fasting level of 13 mU/mL is very common. I see it all the time. And amazingly, even that small elevation in insulin can almost double the growth rate of prostate tissue every year!
So, how do high insulin levels cause such a significant increase in prostate growth? Three ways. One way is that insulin directly promotes prostate growth by interacting with the insulin receptors on prostate cells. Insulin is an anabolic hormone. That means that when it attaches to its receptors on the prostate cells, it acts to double the growth rate. This eventually leads to an enlarged prostate.
The second way is that high insulin levels also lead to lower levels of sex hormone-binding globulin (SHBG). SHBG acts to decrease the ability of androgens and estrogens to interact with prostate cells. Androgens and estrogens act to increase prostate growth just like insulin itself does. So, when the elevated levels of insulin cause a decrease in SHBG, that leads to a greater interaction of the androgens and estrogens on the prostate, which in turn increases prostate growth.
The third way has to do with the fact that as insulin resistance gets worse, the body produces more of the hormone IGF-1 (also known as somatomedin). The “I” in IGF-1 stands for insulin. The “GF” stands for growth factor. IGF-1 is not insulin but is similar enough to insulin that it can bind with the insulin receptors on the prostate. And because it is a growth factor, once IGF-1 binds to the insulin receptor, it stimulates the prostate to grow at a faster rate. This action is completely independent of insulin itself.
That’s why, in two well-controlled epidemiological studies, higher IGF-1 levels were found to be directly associated with a significantly higher risk of BPH. But that’s not all.
Insulin-like growth factor binding protein 1 (IGFBP-1) is a protein that binds up IGF-1 and prevents it from acting on the prostate to enlarge it. Not only does insulin resistance lead to higher levels of IGF-1, it also leads to lower levels of IGFBP-1. That frees up IGF-1 to have an even greater growth-stimulating effect on the prostate.
So, if you are putting up with the symptoms of BPH and have an insulin level over 10 mU/mL, one of the first things you need to do is to get that level down.
How do you do that? The detailed answers are listed in my book The Type 2 Diabetes Breakthrough. But here’s the short list of what increases insulin levels: a diet too high in carbohydrates and too low in omega 3 fats, obesity, nutrient deficiencies, especially zinc, magnesium, chromium, vitamin D, and vitamin C, a lack of proper physical exercise, undiagnosed low-thyroid function, and hormonal imbalances. Obviously, the way to lower insulin levels is to correct these problems. Also, there is one more factor that I need to tell you about.
In men, the most common hormonal imbalance associated with high insulin levels is testosterone deficiency. A recent article proves this.
The authors of the article start off by pointing out that BPH is characterized by inflammation in the prostate, and that this is very common in men with metabolic syndrome. They also logically realized that a man’s prostate is small when he is young and has high testosterone levels and then becomes enlarged as he gets older, when his testosterone levels also get lower. This fact seems to indicate that testosterone deficiency may play a role in BPH.
So, they decided to see if giving testosterone replacement therapy in men with low testosterone levels and metabolic syndrome could reduce prostate inflammation and the symptoms that go along with a swollen prostate. Here’s what they did and what happened.
The researchers enrolled 120 men all of whom had metabolic syndrome and were waiting for surgery for BPH. Of these, 48 of the men had total testosterone and free testosterone levels in the normal range. The other 72 had either a low total testosterone or a low free testosterone. The researchers gave testosterone replacement to half of the men in this latter low testosterone group. They gave the other half a placebo.
Before the study started, all the men filled out symptom questionnaires and had an ultrasound to determine prostate inflammation. After the six months, they repeated the questionnaires and the ultrasounds and then had the scheduled prostate surgery. The researchers then examined the prostate tissue from the surgery for inflammation markers.
The men treated with the testosterone had a “significant decrease in ultrasound markers of prostate inflammation.” Also, the tissue markers of inflammation were significantly lower compared with placebo. As for symptoms, the men treated with testosterone had improvement on one of the questionnaires whereas the men on the placebo had no improvement on either. But what about men with BPH who don’t have metabolic syndrome. Could testosterone therapy help them?
In another paper, the researchers performed an extensive search of all the published preclinical and clinical studies on testosterone therapy and BPH. They concluded that rather than high testosterone being associated with BPH, the “mounting evidence” showed that low levels were the problem. This was especially true when low testosterone levels happened along with high estrogen levels.
They concluded that men with BPH and bladder-related symptoms, regardless of whether or not they had metabolic syndrome, would be able to decrease their symptoms and the inflammation in their prostates with testosterone therapy.
When you add it all up, if you’re a man who has bladder or prostate symptoms, start taking 1 tablet of Advanced Prostate Formula (800-791-3395) twice a day. And if your insulin levels are over 10 mU/mL, please do what it takes to get the levels down into the 7 mU/mL area. You are much more likely to respond to Advanced Prostate Formula with healthy insulin levels.
Also, if you have signs or symptoms suggestive of low testosterone, especially if your testosterone levels are below range, talk to your practitioner about a trial of testosterone therapy. If you can’t find the right practitioner, you can find one on the A4M Find a Doctor page.
Resources
Corona G, Vignozzi L, et aal. Benign prostatic hyperplasia: a new metabolic disease of the aging male and its correlation with sexual dysfunctions. Int J Endocrinol. 2014; 2014:329456.
Rastrelli G, Cipriani S, et al. Testosterone replacement therapy is able to reduce prostate inflammation in men with BPH, metabolic syndrome and hypogonadism: preliminary results from a randomized placebo-controlled clinical trial Endocrine Abstracts (2019) 63.
Rastrelli G, Vignozzi L, et al. Testosterone and Benign Prostatic Hyperplasia. Sexual Medicine Reviews Vol 7, Issue 2, April 2019,
pp259-271
Zhang X, Zeng X, Liu Y, Dong L, Zhao X, Qu X. Impact of Metabolic Syndrome on Benign Prostatic Hyperplasia in Elderly Chinese Men. Urol Int. 2014 May 22.
Originally published in the February 2022 Second Opinion newsletter. Republished with permission.