DigestiveSystemIllustration.jpg
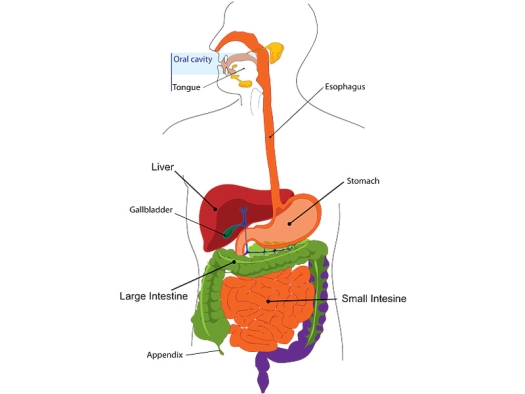
Illustration by Clker-Free-Vector-Images / Pixabay License
It’s safe to say that just about everyone has experienced a tummy ache or digestive upset at one point or another. But what happens when your tummy ache seems to never go away? Or your digestive upset is so bad that it begins interfering with your ability to even get through the day? This is the frustrating and unpleasant reality for a growing number of people struggling with what’s known as inflammatory bowel disease.
But the good news is, that research may be one step closer to understanding and uncovering the secret to potentially healing this perplexing condition. What is this secret? Your microbiome.
Today we’re going to explore exactly what an inflammatory bowel disease is, how this condition is linked to your microbiome, and the monumental impact your diet can have on transforming your gut health. Let’s dive in.
What Is Inflammatory Bowel Disease (IBD)?
Inflammatory bowel disease or IBD isn’t a singular disease, but rather a blanket term to describe a group of disorders that trigger chronic and oftentimes severe inflammation of the digestive tract. The two primary forms of IBD are Crohn’s disease and ulcerative colitis. Crohn’s disease can affect any part of your digestive tract (from your mouth to your anus), while ulcerative colitis is isolated to your large intestine.
The symptoms of inflammatory bowel diseases often wax and wane and can include things like:1
- Abdominal pain and/or discomfort
- Diarrhea and/or constipation (sometimes alternating between the two)
- Bowel urgency (the urgent need to have a bowel movement)
- Bloating and gas
- Loss of appetite or unexplained weight loss
- Blood or mucus in stools
- Nausea and/or vomiting
- Fatigue
- Fever
- Occasionally IBD may cause seemingly unrelated symptoms like joint pain, skin rashes, or vision problems
So what causes these unpleasant and sometimes even debilitating symptoms? The secret may lay in what’s known as your gut microbiome.
What Is Your Gut Microbiome?
Your gut microbiome is the collective ecosystem of microscopic microbes that call your digestive tract home. This complex ecosystem of microbes works together with the cells of your own body to carry out the day-to-day functions that keep you alive and well. Your gut microbiome is designed to maintain a delicate balance – with trillions of different microbes of all different kinds each doing their part.2
But when it comes to the microbes that make up your microbiome, not all of these organisms are created equally. You see, there are some microbes that are harmful and throw off the harmonious balance of your gut microbiome if their populations are left unchecked. When your microbiome is thrown off-kilter by an overgrowth of these not-so-friendly microbes, it leads to what’s known as gut dysbiosis.
And conversely, there are other types of microbes that are particularly beneficial – contributing significantly to keeping your gut happy and healthy. These beneficial strains of microbes are typically specific strains of good bacteria known as probiotics. And understanding the role these different microbes play in your gut is crucial to understanding inflammatory bowel disorders.
Dysbiosis and Inflammatory Bowel Disease (IBD)
Studies have found that an alteration in your gut microbiome that creates dysbiosis can create a domino effect that can contribute to the severe inflammation seen in inflammatory bowel disorders. Exactly how gut dysbiosis can trigger this inflammation and damage to your gut goes something like this:3, 4
- “Bad” bacteria levels spike: In gut dysbiosis, the microbial populations within your gut shift in a way that allows overgrowth of not-so-friendly microbes that crowd out and overpower the “good” bacteria in your gut.
- Immune system mobilization: This shift in your gut microbiome sounds the alarm – activating your immune system. As your immune system responds, it deploys pro-inflammatory chemicals and war-ready immune cells to your digestive tract in an attempt to identify and neutralize the threat. During the process, inflammation levels within your gut steadily rise while your immune system hunts for the perceived threat.
- An increase in intestinal permeability: This influx of pro-inflammatory chemicals paired with gut dysbiosis triggers what’s known as increased intestinal permeability. When your intestinal permeability increases, the integrity of the lining of your gut becomes compromised and forms “gaps” that allow harmful microbes and toxins to “leak” out of your gut. As these molecules leak past your gut barrier and come into contact with the inner layers of your digestive tract, they further activate your immune system – causing inflammation levels to skyrocket.
- Impaired digestion: This combination of gut dysbiosis, increased intestinal permeability, and sky-high inflammation disrupts your gut’s ability to properly break down and absorb vital nutrients – creating a vicious cycle that further enhances this trio of imbalances.
This domino effect is thought to be one of the root causes of inflammatory bowel disease. While the gut bacteria that contribute to gut dysbiosis certainly aren’t limited to a singular species, there is one specific strain of bacteria that has been identified as a potential underlying culprit in inflammatory bowel disease.
Klebsiella and Inflammatory Bowel Disease
Studies have found that a microbe known as Klebsiella may be one of the primary culprits contributing to dysbiosis and subsequent inflammation seen in inflammatory bowel conditions. You see, Klebsiella is naturally present in small amounts in your digestive tract. But a diet high in refined sugars and quickly digested carbohydrates can cause Klebsiella populations to skyrocket.
As Klebsiella microbes proliferate and populate your gut, it triggers your immune system to begin producing antibodies to neutralize the overgrowth. This causes a significant spike in inflammation that can lead to the tissue damage and unpleasant symptoms seen in inflammatory bowel disorders.5
So if these “bad” bacteria like Klebsiella can trigger this intense underlying inflammation, can “good” bacteria flip the script and reverse this underlying imbalance?
Probiotics and Inflammatory Bowel Disease
So, can probiotics help to reverse the underlying dysbiosis and uncontrolled inflammation seen in inflammatory bowel disorders? The answer to that question is – yes! Studies have found that we can in fact modulate the composition of the gut microbiome in a way that can mitigate some of the effects seen in inflammatory bowel disease.
Research has found that, in general, those with inflammatory bowel disorders tend to be deficient in specific strains of beneficial bacteria or probiotics. In particular, they tend to be deficient in strains of probiotics known to produce compounds known as short-chain fatty acids. These short-chain fatty acids serve as a primary food source for the cells that line your gut, known as colonocytes.6
Without adequate production of short-chain fatty acids, these colonocytes can begin to degrade – compromising the integrity of your gut which can spark the vicious cycle of inflammation and dysbiosis. And as it turns out, the best way to support a healthy and thriving population of these short-chain fatty acid-producing probiotics is through your diet.
Is There A Specific Diet for Inflammatory Bowel Disease (IBD)?
While there’s not necessarily a “right” or “wrong” diet when it comes to inflammatory bowel disease, there are certain patterns of eating that can support healing and combat flare-ups. Studies have found that there are specific types of food that can minimize inflammation while promoting the growth of probiotics that help to strengthen the integrity of your gut lining. These specific gut-supporting foods include:7
- Prebiotic-rich foods: Prebiotics are foods high in indigestible fiber that short-chain fatty acid-producing probiotics thrive on and love using as their favorite source of fuel. Some of the best prebiotic-rich foods include any variety of fruits and vegetables as well as oats, and honey.
- Probiotic foods: Probiotic foods are typically fermented foods that contain their own digestible populations of probiotics. Some examples of probiotic foods include kombucha, kefir, sauerkraut, kimchi, and yogurt.
- Beneficial foods: Beneficial foods are foods that combat inflammation and provide the nutrients your gut needs to operate on all cylinders. Some beneficial foods include lean animal protein, vegetable protein, and fatty acids (like monounsaturated fats and omega-3s found in things like olives, nuts, seeds, dark chocolate, and salmon).
On the flip side, there are also some foods that can be potent contributors to inflammation and gut dysbiosis such as:7
- Wheat
- Lactose from processed dairy products
- Animal protein high in fat
- Processed fried animal protein
- Fried vegetable protein
- Artificial sweeteners
- Food and beverages high in refined, processed sugar
- High-fat processed foods
- Corn and some starchy vegetables
Increasing consumption of these gut-supporting foods and avoiding these gut-disrupting foods have been found to have a dramatic effect on both inflammation levels and gut microbiome composition.
Are You Struggling With An Inflammatory Bowel Disease?
Inflammatory bowel disorders can be incredibly frustrating and put a serious damper on your life. While we may not always be able to control the cards we’re dealt, the good news is, we are 100% in control when it comes to the day-to-day choices we make. And one of the most potent ways you can take control of your own health and well-being if you’ve been diagnosed with an inflammatory bowel disorder or are struggling with persistent digestive issues is to prioritize eating a healthy, well-rounded, gut-supporting diet.
If you need help incorporating these healthy foods, I’ve got a whole library of delicious recipes you can check out. And if you need a little extra boost, there are some potent gut-boosting supplements that can help fill in any nutritional gaps. I recommend things like:
- Spore probiotics support microbial diversity
- Gut Calm provides gut soothing ingredients and supports short-chain fatty acid-producing probiotics
- Gut Shield to help beef up the integrity of your gut lining
- Gut Immune powder to support your mucosal immunity and fight pathogens
- Super Turmeric is a full-spectrum product providing antiinflammatory support
Resources
- Inflammatory Bowel Disease: Symptoms, Treatment & Diagnosis (clevelandclinic.org)
- Microbiome (nih.gov)
- Dysbiosis of gut microbiota in inflammatory bowel disease: Current therapies and potential for microbiota-modulating therapeutic approaches | Bosnian Journal of Basic Medical Sciences (bjbms.org)
- Dysbiosis in the Gut Microbiota in Patients with Inflammatory Bowel Disease during Remission | Microbiology Spectrum (asm.org)
- The Role of Klebsiella in Crohn’s Disease with a Potential for the Use of Antimicrobial Measures – PMC (nih.gov)
- Formation of short chain fatty acids by the gut microbiota and their impact on human metabolism – PMC (nih.gov)
- Dietary manipulation of the gut microbiome in inflammatory bowel disease patients: Pilot study (tandfonline.com)
How Transforming Your Diet and Microbiome Can Help Heal Inflammatory Bowel Disease was originally published on Dr. Jill's website on September 7, 2022; used with permission.


