borrelia-burgdorferi-bacteria-13175.jpg
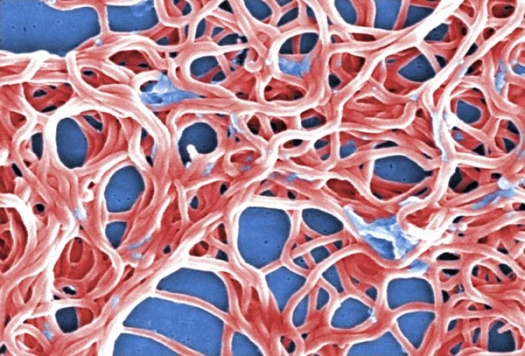
Photo by Janice Haney Carr, ID# 13175, ©2011 / CDC Public Health Image Library (PHIL)
This digitally-colorized scanning electron micrograph depicts a grouping of numerous Gram-negative, anaerobic, Borrelia burgdorferi bacteria, responsible for causing Lyme disease, transmitted through the bite of infected blacklegged ticks.
Until two years ago, Debra Rae was always on the go. She worked full time, was involved with her family’s activities, and enjoyed hiking, snowboarding, Zumba, and mountain biking. Then her health began spiraling downhill.
“Within months, I went from active and healthy to feeling old and frail. My migrating symptoms included stabbing and shooting pain, numbness and tingling, stiffness and spasms, memory and attention difficulties, loss of balance and vertigo, vision problems and sensitivity to light and sound, gastrointestinal and bladder issues, shortness of breath and heart palpitations, skin rashes and night sweats, lack of energy, and more. In short, I was a wreck.
“I saw five doctors, including a neurologist, a rheumatologist, and an orthopedic specialist, and endured physical therapy for 12 weeks. I received about 50 pages of test results from X-rays, MRIs, and EMGs to blood and urine tests to rule out vitamin deficiency, heavy metal toxicity, hepatitis, lupus, rheumatoid arthritis, thyroid issues, and brain and spinal damage. No one was able to give me a diagnosis. My life was in shambles. I wasn’t able to do any of the activities I loved doing. I couldn’t even wear shoes because the pain was so bad.
“Then I went to Whitaker Wellness. My physician immediately suspected Lyme disease, even though I could not remember ever having a tick bite. My tests came back positive, and he started me on antibiotics along with supplements and IV therapies to boost my immune system and reduce symptoms.
“Diagnosing Lyme disease and guiding me on the path to health has dramatically changed my quality of life. The pain is much better, and I can now wear shoes. My thinking is clearer, and I am reading again. I have more energy, and I am able to do chores, walk the dog, and take my son to soccer practice. We are going to Utah soon, and I am planning on snowboarding, which I haven’t been able to do for a very long time.”
Beyond the Obvious
Everybody knows about Lyme disease. It’s an infection transmitted by deer ticks in wooded areas of the Northeastern US that causes a red bulls-eye rash and flu-like symptoms and is treated with antibiotics, right?
Yes and no. Lyme disease is caused by a bacterial infection, Borrelia burgdorferi, although many patients are also infected by other tick-borne pathogens that may cause even more problems. Infected ticks are not limited to the Northeast but are found throughout the US. More than 300,000 Americans are infected every year—10 times more than previously believed.
Only 50 percent of individuals infected with Lyme report the characteristic bulls-eye rash, and a similar number don’t recall a tick bite at all. Symptoms can run the gamut from transitory fever and achiness to severe, enduring, and debilitating pain and dysfunction affecting systems throughout the body.
The usual treatment is a two to four-week course of antibiotics, which may be effective, especially if the infection is diagnosed and treated right away. However, as many as 40 percent of patients end up with lots of chronic problems—Debra is a textbook case—and consult multiple doctors and suffer for years before getting a proper diagnosis.
Misdiagnoses, unfortunately, are all too common. Patients may be told they have autoimmune disorders, chronic fatigue, fibromyalgia, Parkinson’s, even hypochondria or other psychological problems. As a result, they may be treated with intensive, expensive drugs that have no chance of helping and actually make them worse.
Lyme Wars
The truth is, Lyme disease is in many ways a mystery. Conventional diagnostic lab tests are notoriously unreliable, and huge schisms exist in the medical community about how it should be treated.
In one corner of the “Lyme wars” is the large and influential Infectious Diseases Society of America, which contends that chronic, long-term Lyme infection doesn’t even exist. In the other corner are physicians who are willing to use more sophisticated testing and treat their patients with alternative therapies such as IV nutrients, hyperbaric oxygen, immune-boosting supplements, and/or longer and varying antibiotic regimens.
Unfortunately, insurance companies often refuse to pay for “experimental” tests and treatments, and innovative doctors who treat Lyme disease are sometimes shunned or harassed by their conventional colleagues and medical boards.
Controversial or not, when a patient like Debra comes to Whitaker Wellness with a slew of symptoms or a diagnosis of Lyme disease, we’re going to do our best to get the bottom of it and find a solution.
“A New Lease on Life”
We use cutting-edge lab tests to look for various strains of Borrelia and other infectious agents and follow the latest antibiotic protocols for targeting specific bacteria. We treat patients with intravenous therapies, such as glutathione, minerals, and vitamins, including vitamin C, which has direct antimicrobial activity. Because Borrelia thrives in a low-oxygen environment, hyperbaric oxygen therapy, which saturates the system with oxygen, is another good treatment.
Medicinal herbs and nutritional supplements that support the body’s ability to fight infection, and low-dose naltrexone, a proven immune enhancer, are also cornerstones of our Lyme disease treatment program.
Finally, we address our patients’ pain and diverse symptoms with the safe, effective therapies Whitaker Wellness is known for: neurofeedback for cognitive problems, EECP for vascular issues, and high-intensity laser, acupuncture, and PRP for pain, to mention a few.
Its high time physicians and insurance companies pull their heads out of the sand and help, rather than hinder patients by acknowledging chronic Lyme disease for what it is: a very real and difficult condition that cannot be cured overnight.
After more than two years of misdiagnoses and inappropriate treatment, Debra can tell you there is hope for chronic Lyme disease. “Although it is a slow recovery, I am finally headed in the right direction. Every day, I get back a little piece of my former self, and I will be forever grateful for a new lease on life.”
To learn more, visit Dr. Whitaker's website
References
Adrion ER, et al. Health care costs, utilization and patterns of care following Lyme disease. PLoS ONE. 2015 Feb 4;10(2): e0116767.
Cameron DJ, et al. Evidence assessments and guideline recommendations in Lyme disease: the clinical management of known tick bites, erythema migrans rashes and persistent disease. Expert Rev Anti Infect Ther. 2014 Sep;12(9):1103–35.